Osteochondrosis is one of the most common diseases today, often affecting women over 25 years of age. The disease is characterized by an acute, rapid course when comparing the course of the disease, especially in male patients.
The pathological processes accompanying the disease are the destruction of articular tissues, intervertebral discs. In 30% of cases, the cause of the headache is pathology. If a woman develops symptoms of cervical osteochondrosis, you should see a doctor immediately, as this will help prevent the disease from developing further.

What is cervical osteochondrosis
Osteochondrosis is a chronic disease that is accompanied by damage to one or more parts of the spine. Depending on this, the clinical manifestations of the disease differ.
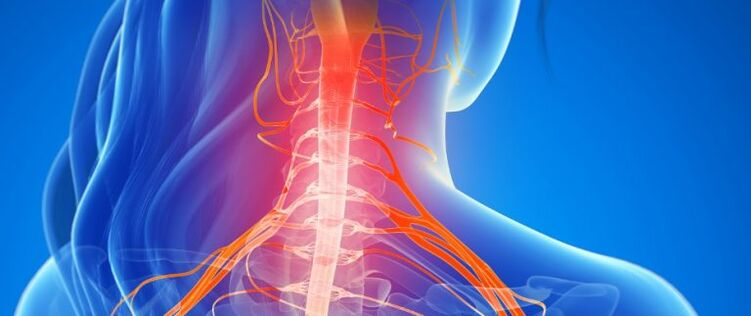
The main load falls on the lower back, but there are more problems with the defeat of the cervical region. This is due to the anatomical features of the body, there are many fibers and nerve endings in the cervical region, and there are blood vessels in the brain on which the blood circulation depends.

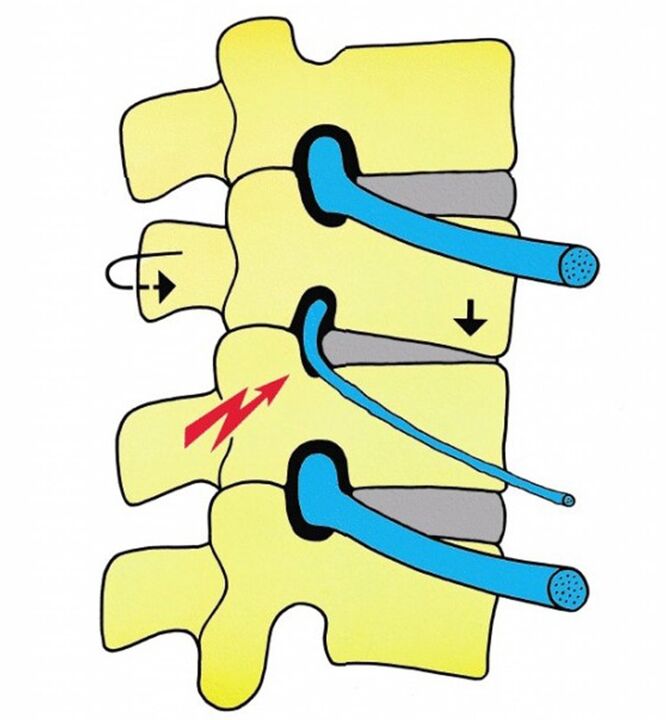
The cervical region is considered more sensitive due to the proximity of the vertebrae and the proximity to the arteries involved in the delivery of nutrients to the brain. Displacement of the vertebrae causes constriction of nerve roots and arteries, followed by changes in the intervertebral cartilage, the development of hernias and protrusions. These changes in the intervertebral discs are often age-related, and the disease can manifest itself at a young age.
Predisposing factors
There are many reasons for the development of cervical osteochondrosis in women, the predisposing factors include:
- taking hormonal drugs - it causes metabolic disorders;
- increased load on the spine and spinal muscles (develops as a result of improperly organized workplace, in hazardous industries or lifting weights, engaging in professional sports);
- dietary disorders, consumption of harmful foods, lack of nutrients;
- insufficient water intake (clean, without harmful additives and impurities) - it leads to drying of cartilage tissues, ligaments, which clogs the body with toxins;
- low physical activity - against the background of lack of physical exercise there is a violation of blood circulation in the muscles, insufficient nutrition of the intervertebral discs;
- genetic predisposition, congenital curvature of the spine;
- previous diseases (arthritis, osteoarthritis, neuralgia, vasospasm, etc. );
- transplanted spinal injuries;
- constant stresses - they are often psychosomatic in nature, uncontrolled muscle contraction occurs against the background of tension, resulting in circulatory processes, slowing of lymph flow, deposits of toxins and toxins are observed.

Secondary risk factors:
- incorrect position of the spine during sleep and rest, incorrect choice of mattress and pillow;
- sleep without a pillow;
- pregnancy;
- overweight.
Age - as the body ages, the vertebrae wear out, the cartilage tissue wears out, the calcium is washed away, the body weight is not properly distributed to the legs, and there is an uneven load on the spine.
Symptoms of cervical chondrosis in women
Cervical osteochondrosis can be asymptomatic for a long time, many associate limited motor activity with fatigue, and pain is rare in the early stages of the disease.

The onset of pain is often associated with poor sleep and often stress. In some cases, the symptoms of normal cervical osteochondrosis appear very quickly in women. The day before, a woman may feel well, and the next day, severe pain prevents her from moving freely until she can lift her head from the pillow. This condition is a reason to seek medical attention, at this stage you can easily cope with the symptoms of the disease.
General symptoms of the disease
In women, the symptoms of the acute stage of cervical osteochondrosis are more pronounced. Cartilage puts pressure on the nerve roots, puts pressure on the blood vessels that run along the spine. There is a risk of short-term memory loss, often due to oxygen starvation. Lack of therapy can cause paralysis when there is pain, numbness in the shoulder area, tingling in the fingers and other symptoms.

Reflex syndrome
In women, manifestations of cervical osteochondrosis are often associated with reflex syndromes, the symptoms of which occur against the background of constant irritation of the spinal cord receptors, as a result of which the neurons become reflexively excited.
This leads to malnutrition, metabolic processes, as well as constriction of blood vessels and nerves.
Reflex syndromes are divided into:
- Painful - back pain, neck pain, simultaneous pain in the back of the head, neck, shoulder / forearm.
- Muscle tonic - results in constant muscle tension, oxygen starvation, swelling, sealing.

Spasms can also occur periodically in the muscles of the head, cervical region and shoulder girdle.
In the early stages of the disease, syndromes of the lower oblique muscle of the head, scapular-costal syndrome, vertebral artery syndrome, skeletal muscle tension often occur.
radicular syndrome
Radicular syndrome often occurs in women with cervical lumbar osteochondrosis, accompanied by constriction of the nerve roots of the spinal cord. Disorders of movement in pathological hands are accompanied by loss of sensitivity. In this case, there are disorders of the internal organs (pathology of urination, sexual dysfunction, hypertension, memory impairment). Damage to blood vessels can occur unexpectedly with sudden movements in the affected area.
Vascular syndrome
Against the background of symptoms of compression of cerebral vessels, women develop a symptom of osteochondrosis of the cervical spine, in extreme cases, develop ischemic stroke. This complication is accompanied by impaired motor function of the extremities, decreased sensitivity, deterioration of the internal organs. Sometimes the organs stop working and if the kidneys fail, the chances of death are high.
Stages of development of osteochondrosis
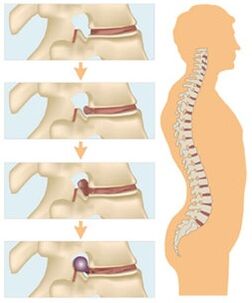
There are four stages of the disease, all of which are accompanied by certain pathological changes.
1st stage
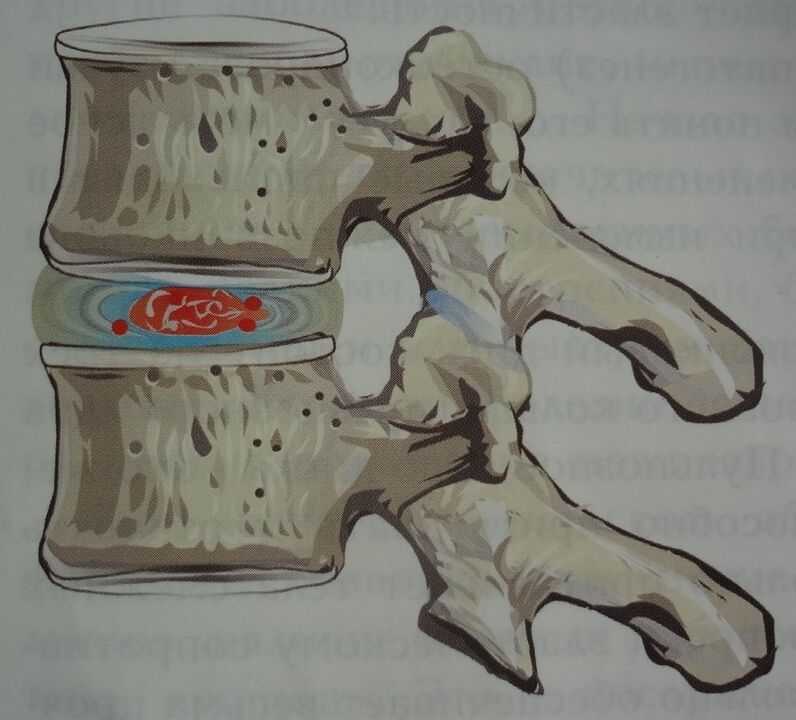
In the first stage of the disease, damage to the pulp nucleus of the intervertebral disc is observed. This phenomenon occurs against the background of disruption of metabolic processes in the body, as a result of dehydration, the nucleus dries up, shrinks in size and becomes less durable. The spine is more sensitive to physical stress, there is no pain syndrome at this stage. Diagnosis at this stage does not require medication.
Stage 2
At this stage, the fibrous ring is damaged, and tears and fissures form on the surface of the intervertebral disc due to the loads falling on the spine. The ring becomes thinner, the core is transferred to cracks and fissures, which causes them to expand. The enlarged disc extends beyond the vertebrae, the disc protrudes, and the process is accompanied by pain.
3 stages
With third-degree osteochondrosis, an intervertebral hernia is formed, and the fibrous ring is torn. The pulposus nucleus moves into the subglottic cavity, resulting in a disc herniation. The pathological process causes damage to nearby blood vessels, muscle tissue, ligaments and nerves.
4 stages
This stage is accompanied by degenerative recovery of the spine, which lasts up to 12 months. During this period, the nature of bone growth changes, they begin to grow in width, which leads to an increase in the area of the vertebrae. Thus, the formation of osteophytes occurs, as a result of which the mobility of the spine decreases, destructive processes stop.

Methods of treatment
Treatment of any stage of cervical osteochondrosis in women should be aimed primarily at eliminating the causes of the disease. Therapy should be comprehensive, this approach will help prevent further spread of the pathological process.
The course of treatment should focus on the restoration or activation of lymph flow and venous flow from the affected areas. Maintaining a healthy lifestyle is an excellent prevention and treatment of cervical osteochondrosis. Painkillers are indicated as part of first aid, and NSAIDs are highly effective.
After first aid, you should consult a doctor, who will help you determine the right treatment.
Medical
The following drugs are prescribed for the treatment of osteochondrosis:
- Non-steroidal anti-inflammatory drugs (tablets, injections) - their action is aimed at reducing pain and eliminating the inflammatory process. Therapy can take several months, but they adversely affect the functioning of the gastrointestinal tract.
- Steroid anti-inflammatory drugs (hormones) - prescribed for severe pain. They are effective in relieving inflammation and pain, but also have side effects in the form of adverse effects on the gastrointestinal tract.
- Antispasmodics - effectively relieve muscle spasms, have a relaxing effect on muscles, activate circulatory processes.
- Epidural blockade - the introduction of painkillers and hormones into the space between the meninges and the periosteum of the vertebrae during its implementation.
The use of chondroprotectors, muscle relaxants is also indicated as part of the treatment of osteochondrosis, the dose and duration of therapy is determined by a physician.
Gymnastics
For women with symptoms of cervical osteochondrosis, it is recommended to perform physiotherapy exercises in accordance with the doctor's instructions. All movements should be discussed with a specialist, as incorrect placement of the neck and arms can aggravate the situation.
Effective neck exercises:
- Extend the arms to the sides, lift them up with light turns of the body. The right palm should reach the left and vice versa, repeat 5-6 times.
- Stretch your arms across your body, stretch your abdomen, try to relax your muscles, turn your head in different directions in turn. The edges of the ears should touch the ground, do 10 repetitions.
- Stand up straight with your shoulders straight, slowly turn your head in different directions, repeat 6-7 times.
- Tie the elbows together, tying the fingers at the back of the head, tie the chin to the front arms, repeat 6-7.
It is recommended that all exercises be performed regularly, only in this case the effectiveness of therapy is achieved.
Physiotherapy and massage
Compression of the spine is accompanied by severe pain, the doctor prescribes physiotherapeutic methods to eliminate the pathological manifestations of the disease. Their action is aimed at relieving pain, reducing anxiety and activating circulatory processes.
The following physiotherapeutic methods are most commonly prescribed for osteochondrosis:
- shock wave therapy;
- electrophoresis;
- acupuncture;
- laser therapy;
- balneotherapy;
- massage.

Massage is effective in relieving pain, resulting in lost mobility. Physical exposure to the affected area activates circulatory processes, reduces tone, strengthens muscles. The application of the method minimizes the risk of pathological processes in the future.
Different massage methods are used during treatment, much depends on the clinical picture, the characteristics of the patient's body, the stage of the disease.
There are contraindications to massage, which should be considered before prescribing the procedure. In case of vascular pathologies, high blood pressure, injuries, skin inflammation, you need to be careful.
Food
Diet plays an important role in osteochondrosis, it should be balanced, it is better to contact a nutritionist. Consumption of salty foods and mineral water should be minimized. It is recommended to eat in small portions 5-6 times a day, fried, baked, spicy foods should be replaced by steamed foods. It is recommended to give preference to protein products (legumes, dairy products), chondroitins, sprouted grains, sesame seeds. Prohibited coffee, alcohol, strong tea.

Alternative treatment
It is also recommended to use alternative therapies in conjunction with traditional methods. A doctor's consultation is required first. Such methods can reduce the severity of symptoms, but do not eliminate the cause of the development of the pathological process. Ointments, infusions, decoctions, compresses, rubs, baths are widely used as part of folk medicine. In their production, various herbs, alcohol, oils, honey, etc.
Effective recipes:
- Put a handful of chopped celery in 200 ml of boiling water, insist 5 hours, drink 1 tablespoon of the filtered mixture. l. daily.
- Heat burdock or horseradish green leaves in a steam bath, apply for an hour.
- Mix honey and fried potatoes in equal proportions, use the mixture for compresses.

Therapeutic baths
The effect of therapeutic baths:
- thermal - under the influence of high temperatures, circulatory processes are accelerated, intensified, the sensitivity of receptors increases, enzymes are activated, inflammatory processes are reduced;
- mechanical - blood circulation is activated under water pressure, as a result of which tissues are saturated with oxygen and nutrients;
- After the addition of chemicals - salt, minerals, herbs, water acquires healing properties, baths also have a stimulating effect on the excretory system, resulting in increased resistance of the body to disease.
Coniferous, salt, mustard baths are highly effective, the duration of the procedure is 20-30 minutes. It is recommended to sleep in a warm bed after the session, as the cold can nullify all the effects of therapy. The procedure should be discontinued if there are problems with cancer, heart or blood vessels.


















